
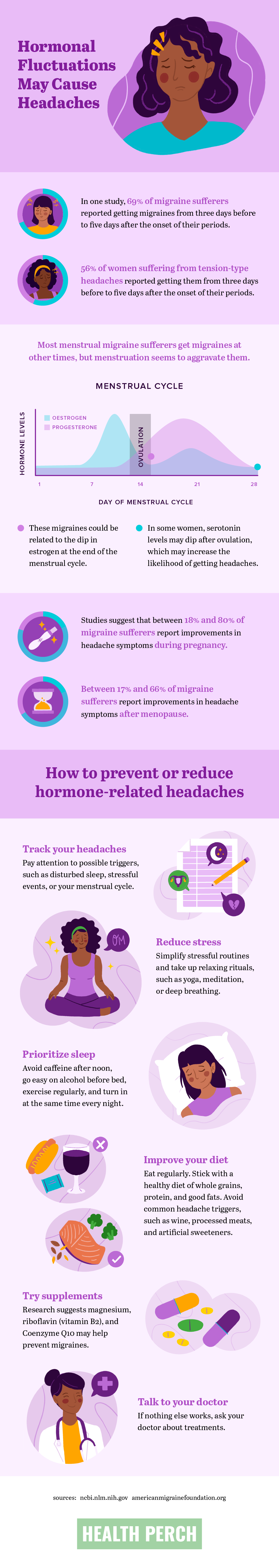
Aching, stabbing, or pounding: Whatever way your head hurts, it’s not fun, and it’s not uncommon. About 50 percent of the world’s population suffers from headaches every year. And women experience about twice as many headaches as men. Why? Fluctuating hormones may be the culprit.
Read on to learn more about why hormonal headaches are so common and what women can do about them.
Common types of headaches
Most headaches fall into one of four common categories.
Tension headaches
The most common types of headaches are tension headaches, which disproportionately impact women. People usually feel tension headaches on both sides of the head. They can feel like a tight band encircling your head or a dull, aching pain. Tension headaches may be caused by stress as well as tightness in the neck, shoulder, and scalp muscles.
Migraines
Migraines also disproportionately impact women, usually by a factor of about two to one. You may feel migraines as throbbing pain or a pulsing sensation, often limited to one side of the head. In addition to headaches, migraines can cause nausea, vomiting, and sensitivity to light and sound. They tend to be more severe than tension headaches and can interfere with daily activities. Hormonal changes are a major trigger for migraines, but other factors — such as stress, sleep changes, and physical exertion — may trigger migraines.
Cluster headaches
Less common than tension headaches or migraines, cluster headaches are characterized by brief but severe headaches focused in or around one eye. Other symptoms may include tearing and redness of the eye, runny or stuffy nose, and a drooping eyelid. Hormones or stress generally don’t trigger these headaches, and they impact men more frequently.
Medication-overuse headache
The medications used to treat headaches can cause headaches if overused. If you take pain relievers or migraine mediations more than 10 times a month, you may experience frequent headaches. They may even wake you up in the morning nearly every day. These types of headaches generally eventually stop when you cease taking pain medication.
Which types of headaches are linked to hormones?
Women commonly experience tension headaches before menstruation. Many stressors may contribute to tension headaches, making it difficult for scientists to determine whether tension headaches are caused by hormones or by other events that tend to peak around the time a woman’s period starts.
The connection between hormones and headaches is much clearer with migraines, with up to 70 percent of migraine sufferers associating their menstrual cycle with the onset of symptoms. Migraines are related to changes in the levels of estrogen, which fluctuate during a woman’s cycle. After ovulation, estrogen levels begin to dip, reaching their low right before the start of your period, when migraines tend to occur. Some women also experience a dip in serotonin levels after ovulation, which may contribute to migraines.
Scientists haven’t linked cluster headaches and medication-overuse headaches to hormonal fluctuation.
How to prevent hormonal headaches
Use these tips to prevent and reduce your hormone-related headaches.
Know your cycle
Take some time to understand your triggers. Keep a journal noting when you get a headache, and list what you were doing for the 24 hours before its onset. Did you double up on coffee? Go to bed late or wake up early? Have a stressful day at work? Also note where you are in your cycle. Over time, you may notice patterns not just around your cycle, but around other triggers as well.
Reduce stress
Stress is a common trigger for migraines. Although easier said than done, reducing stress can also reduce your hormonal headaches. Can you simplify some of the most stressful parts of your days? If it’s not possible to eliminate stressors, coping and relaxation strategies — such as meditating, doing yoga, deep breathing, or getting a massage — can help you manage stress.
Prioritize sleep
Although it’s easy to let sleep slide in favor of finishing up a project or catching up with a friend, it’s not always best for your health. Disturbed sleep or lack of sleep are common triggers for hormonal headaches. To get a good night’s sleep, avoid caffeine and alcohol late in the day, exercise regularly, and go to bed at the same time every night. If you’re tired even after consistently sleeping for seven to nine hours per night, speak with your doctor.
Improve your diet and boost nutrition
Keeping a healthy diet rich in whole grains, protein, and good fats can help keep migraines at bay. Be sure to eat regularly; skipping meals or waiting too long between meals can cause headaches or make them more severe.
In addition, certain foods and drinks are known migraine triggers. These include caffeine, red wine and other alcoholic beverages, artificial sweeteners, chocolate, and certain processed meats. Keep a food diary to help you understand whether these or other foods trigger your headaches.
Try supplements
Certain supplements may help prevent hormonal headaches. Multiple studies have shown that some natural supplements such as magnesium, riboflavin (also known as B2), and a co-enzyme called Q10 can help with migraines.
Talk to your doctor about headache treatments
Your doctor may be able to prescribe medication to prevent or manage the pain of your headaches. If you’ve been self-dosing with over-the-counter medication frequently, keep in mind these may contribute to headaches. Your doctor can advise you on how to stop taking these medications.
Conclusion
If you struggle with frequent hormone-related headaches, remember, you’re not alone. Take charge of your cycle and try the tips above to help prevent headaches or at least reduce the number of days you spend with an aching, throbbing, or pounding head.
